ENCINITAS, CA – April is National Minority Health Month, and the American Red Cross is raising awareness about health disparities that disproportionately affect ethnic and racial minority populations.
The Red Cross, which supplies about 40 percent of the country’s blood, reminds blood and platelet donors of the importance of maintaining a stable blood supply this spring to ensure that all patients have access to the blood products they need. United States.
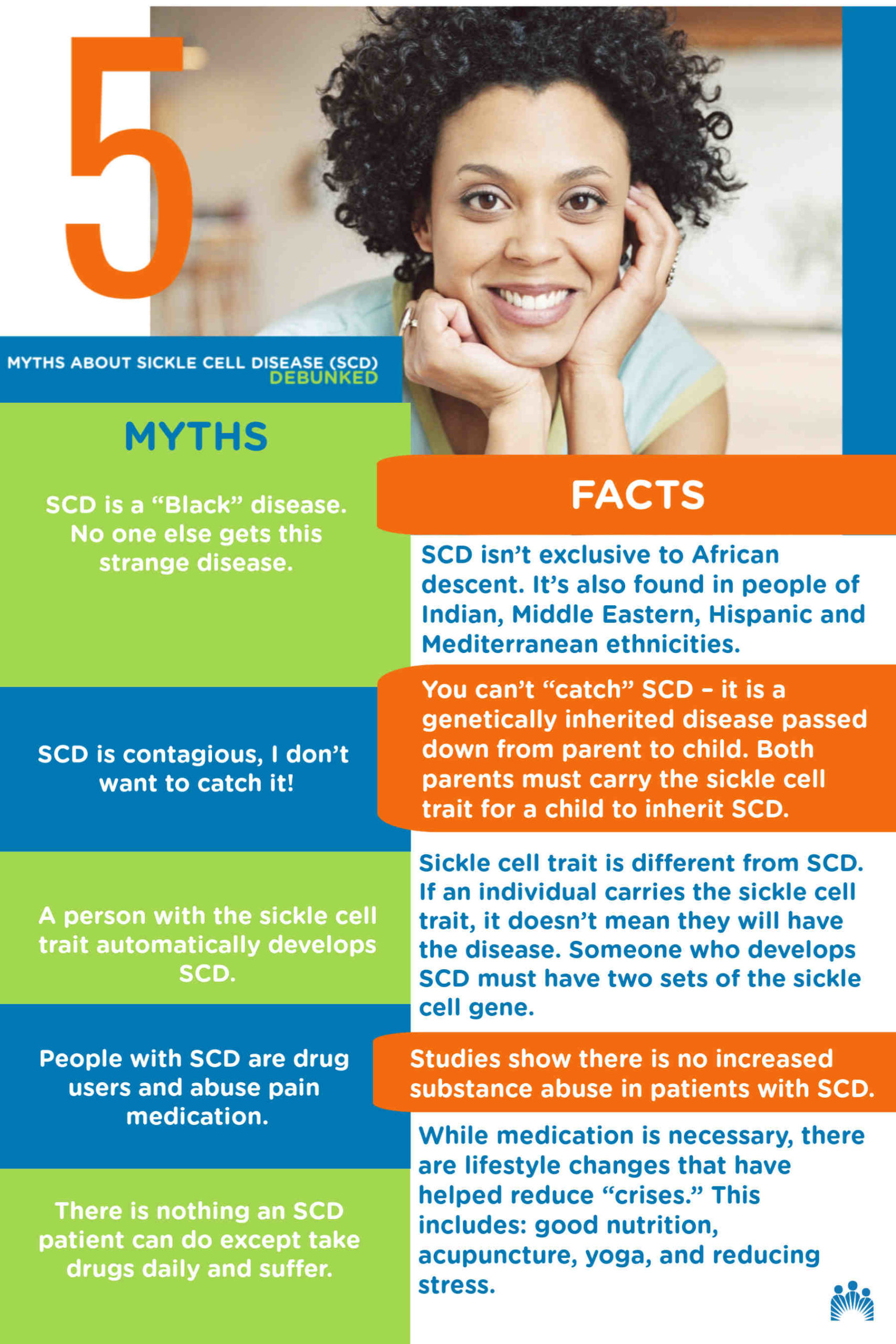
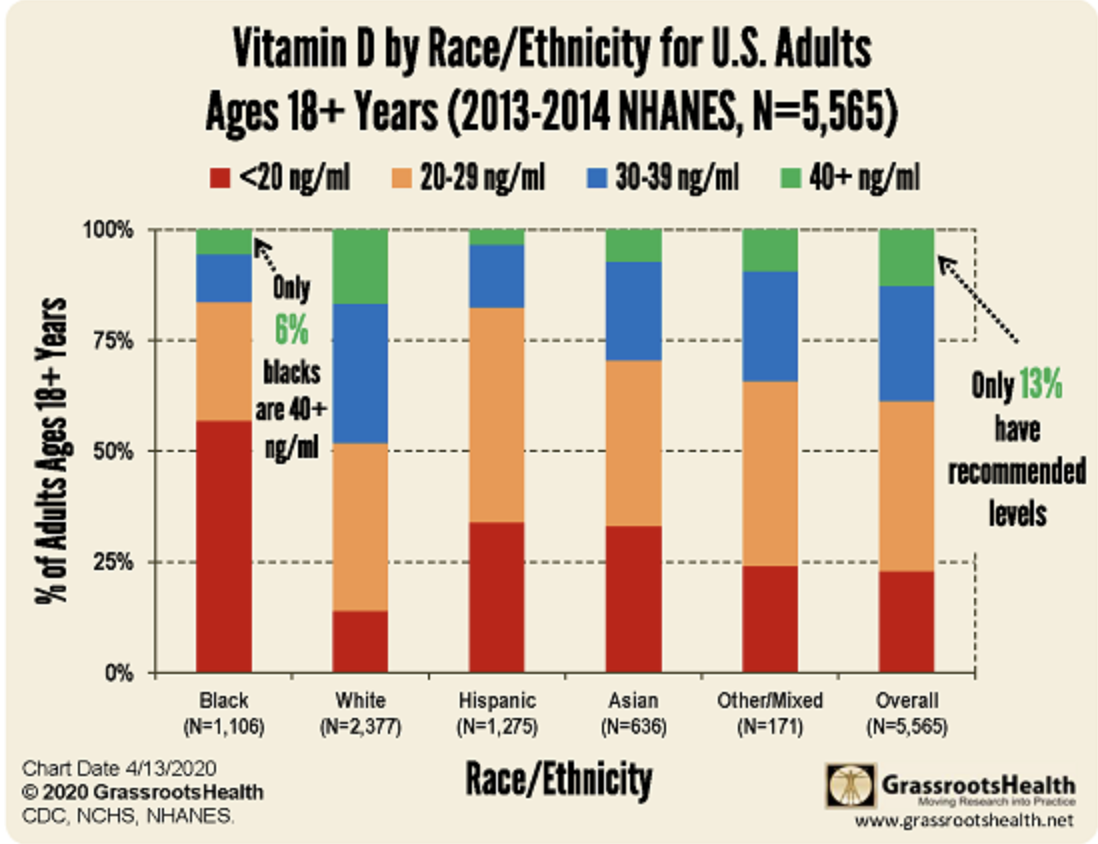
“Blood transfusions remain one of the most critical treatments for patients such as those living with sickle cell disease, most of whom are of African and Latino descent, and major beta thalassemia, which disproportionate to those of Asian descent, “a Red Cross press release said. dit. “In addition, black women are more likely than white women to have severe postpartum hemorrhage, which often requires a blood transfusion.”
Find out what’s happening in Encinitaswith free, real-time updates from Patch.
Anyone donating blood or platelets until April 18 will receive a Red Cross T-shirt, while supplies last. Those who donate between April 19 and May 19 will receive a $ 10 e-gift card from a merchant of their choice and will automatically sign up to win a new caravan.
Red Cross blood is being collected in San Diego County, including Encinitas. See a list of upcoming blood draws below. Donors are asked to schedule an appointment before reaching a blood drive.
Find out what’s happening in Encinitaswith free, real-time updates from Patch.
Blood Donation Opportunities
Kearny Mesa Red Cross Blood Donation Center, 4229 Ponderosa Ave., Suite C (see RedCrossBlood.org for hours)
What To Know About Giving Blood
All types of blood are needed. Are you interested in making a donation? Download the Red Cross Blood Donor App, visit RedCrossBlood.org, or call 1-800-RED CROSS (1-800-733-2767) for more information or to make an appointment.
A blood donor card or driver’s license or two other forms of identification are required at check-in.
People who are 17 in most states (16 with parental consent when permitted by state law) weigh at least 110 pounds and are generally in good health may be eligible for blood donation. High school students and other donors 18 years of age or younger must also meet certain height and weight requirements.
Donors can save time using RapidPass to complete the pre-donation reading and online health history questionnaire, on the day of the donation, before reaching the blood collection.
The rules of replying:
What does antepartum care mean?

Prepartum care, also called prenatal care, is the comprehensive management of patients throughout their pregnancy. Prenatal care has become the most widely used health care service in the United States, averaging more than 50 million visits a year.
How long can a patient live with sepsis?
Many patients are known to die in the months and years after sepsis. But no one knows whether this increased risk of death (between 30 days and 2 years after sepsis) is due to the sepsis itself, or to the pre-existing health conditions the patient had before acquiring the sepsis. complication.
What is the life expectancy after sepsis? Patients with severe sepsis have continued high mortality after severe sepsis with only 61% surviving five years. They also have a significantly lower physical quality of life compared to the population standard, but mental quality of life scores were only slightly below the population standards for up to five years after severe sepsis.
What is the last stage of severe sepsis?
Stage 3: Septic shock About half of patients who develop septic shock will die as a result, according to the Mayo Clinic (2021). There are other complications that can develop from severe sepsis or septic shock. Small blood clots can form all over the body, blocking blood flow and oxygen to vital organs.
What are the chances of survival with sepsis?
As sepsis worsens, blood flow to vital organs, such as the brain, heart, and kidneys, deteriorates. Sepsis can cause abnormal blood clotting that causes small clots or blood vessels to rupture, damaging or destroying tissues. Most people recover from mild sepsis, but the septic shock mortality rate is about 40%.
Can sepsis be completely cured?
Due to problems with vital organs, people with severe sepsis are likely to be very ill and the disease can be fatal. However, sepsis is treatable if it is identified and treated quickly, and in most cases leads to a complete recovery without lasting problems.
How long do you live after sepsis?
Patients who survive severe sepsis have a higher risk of mortality than the general population of the same age for at least 4 years. Several studies have suggested 30-day mortality rates between 30% and 50% for patients with severe sepsis or septic shock.
Does sepsis shorten your life?
Patients who survive severe sepsis have a higher risk of mortality than the general population of the same age for at least 4 years. Several studies have suggested 30-day mortality rates between 30% and 50% for patients with severe sepsis or septic shock.
Can you fully recover after sepsis?

Most people recover completely from sepsis. But it can take time. You may continue to have physical and emotional symptoms. These can last for months, or even years, after having sepsis.
What are some of the symptoms of COVID-19 post-acute sequelae? People with post-acute sequelae of COVID-19 often have difficulty concentrating and memory problems, sometimes referred to as “brain fog.” This deterioration is a common symptom in those with severe fatigue for any reason.
Is it possible to have lingering symptoms of COVID-19?
“Some symptoms of COVID-19 last longer than others,” says Dr. Septimus. “In particular, fatigue and loss of taste and smell may persist beyond the period of infection.” Although uncomfortable and / or uncomfortable, Dr. Septimus adds that these persistent symptoms are not too worrisome for most people.
What is the difference between people who have asymptomatic or pre-symptomatic COVID-19?
Both terms refer to people who have no symptoms. The difference is that “asymptomatic” refers to infected people but never has any symptoms, while “pre-symptomatic” refers to infected people who have not yet developed symptoms but who present them later.
What are the organs most affected by COVID‐19?
The lungs are the organs most affected by COVID-19
What is post-acute COVID-19 syndrome?
Post-acute COVID-19 is a syndrome characterized by the persistence of clinical symptoms beyond four weeks from the onset of acute symptoms. The Centers for Disease Control (CDC) has formulated “post-Covid conditions” to describe health problems that persist for more than four weeks after being infected with COVID-19
Who are at higher risk of developing serious illness from COVID-19?
Older people and those with underlying medical problems such as cardiovascular disease, diabetes, chronic respiratory disease, and cancer are more likely to develop serious illnesses.
What are the complications of COVID-19?
Complications may include pneumonia, acute respiratory distress syndrome (ARDS), multiorgan failure, septic shock, and death.
What are some of the persistent symptoms of COVID-19?
The most common persistent symptoms reported in the follow-up survey were fatigue and loss of taste or smell, both reported among 24 patients (13.6%). Other symptoms include brain fog (2.3%).
Does sepsis have a smell?
Observable signs that a provider may notice during the evaluation of a septic patient include poor skin turgidity, odors, vomiting, inflammation, and neurological deficits. The skin is a common gateway for various microbes.
What are the red flags of sepsis? Warning signs include high fever, low blood pressure, fast heartbeat, difficulty breathing, drastic change in body temperature, worsening of the infection, mental deterioration, and serious illness.
Can sepsis go undetected?
A major and growing threat to the elderly, sepsis can go unnoticed or misdiagnosed. And as patients age, they are more susceptible not only to this life-threatening disease, but also to the chronic diseases associated with sepsis.
Does sepsis always show up in blood work?
Sepsis is often diagnosed by simple measures such as temperature, heart rate, and respiratory rate. You may need a blood test. Other tests can help determine the type of infection, where it is found and what bodily functions have been affected.
How often is sepsis missed?
In a telephone survey of more than 1,000 doctors in hospitals in Europe and the United States, half of whom were specialists in intensive care, 86% said that the symptoms of sepsis could easily be attributed to other conditions. 45% considered that sometimes they have been lost. a diagnosis of sepsis [20].
What are the 6 symptoms of sepsis?
These may include:
- feeling dizzy or faint.
- a change in mental state, such as confusion or disorientation.
- diarrhea.
- nausea and vomiting.
- he speaks confused.
- intense muscle pain.
- severe difficulty breathing.
- Less urine output than normal, for example, not urinating for a day.